For people in low-income communities, medical problems can be caused and worsened by factors related to poverty, such as poor nutrition, lack of safe and stable housing, incarceration, unemployment, and the chronic anxiety of income insecurity. These factors, coupled with a fragmented delivery system where services are provided in a siloed fashion and providers are unable to communicate regularly to coordinate care, mean patients with complex needs face a range of obstacles when seeking health care.
To address these challenges and take a more active role in addressing the state’s homelessness crisis, the California Department of Health Care Services (DHCS) launched the Whole Person Care (WPC) pilot as part of the 1115 Medicaid waiver. Launched in 2016 across 25 sites in the state, WPC is based on the premise that the best way to care for people with complex needs is to address their full spectrum of care, including medical, social, and economic needs. A primary goal of WPC is to build partnerships and develop infrastructure to coordinate care seamlessly across providers from multiple sectors to provide tailored, integrated care for high-risk individuals to improve health.
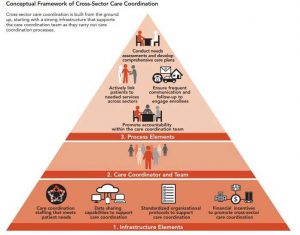
Now, three years into implementation, researchers from the UCLA Center for Health Policy Research released an interim report focused on WPC’s efforts to improve care coordination. They used a two-part framework to assess cross-sector care coordination, focusing on infrastructure and processes. To evaluate pilots’ infrastructure, the researchers assessed staffing needs, data sharing capabilities, standardized protocols, and financial incentives. Care coordination processes were assessed using criteria such as frequent communication, needs assessments, comprehensive care plans, patient linkage to services, and protocols to promote accountability among teams.
While the 25 WPC pilots use very different approaches, the findings suggest that, overall, WPC has resulted in significant improvements in cross-sector coordination for high-risk patients. Two CAPH/SNI members, Contra Costa Health Services and Ventura County Health Care Agency, stand out for offering many of the promising care coordination elements identified in the framework.
Contra Costa’s WPC pilot, CommunityConnect, implemented nearly all of the infrastructure elements in the framework. For example, CommunityConnect developed data sharing agreements between 11 WPC partner organizations, including the County Employment and Human Services agency, to share clinical, social, and eligibility data, and to house that information in a single shared care plan, accessible at point of care.
“Much like an A1C value is vital in supporting diabetes health, housing status and access to CalFresh benefits are essential in supporting stability and holistic wellness. Establishing data sharing agreements with partners is the first step in moving towards that desired state of delivering better and more integrated care to patients,” said Sue Crosby, Whole Person Care Director. “As the healthcare industry rapidly evolves to address social determinants, IT strategy must also evolve to ensure this key information is available for use by the entire care team, at point of care.”
Ventura County’s WPC pilot implemented all of the framework’s process elements, highlighting their robust care coordination efforts. With over 38 partner organizations, Ventura County’s WPC pilot has helped high-risk patients receive timelier and better care. To facilitate warm handoffs between health care and social service providers, care coordinators use active referrals to guide patients to needed services, including scheduling appointments, arranging follow-up after hospital visits, coordinating transportation, attending appointments with patients as their advocate, and assisting with applications for housing, employment, and benefits programs.
“For patients with complex social and medical needs, we have seen a lot of success with our active referral process, where care coordinators serve as a bridge between the patient and provider or system to arrange care, playing a more active role in the process than you’d find in a typical referral or hand-off,” said Deanna Handel, Whole Person Care Manager. “This allows for better monitoring of patient progress, and ultimately, better coordinated care.”
Overall, the findings from the UCLA report suggest that WPC has led to broad improvements in care coordination. Many WPC pilots made great strides in hiring care coordinators and sharing data across sectors, despite multiple challenges, and establishing care processes to engage patients, including comprehensive care plans and actively linking patients to services.
Looking ahead, it will be critical that counties and partners continue to develop the infrastructure to support cross-sector care coordination, especially as WPC sunsets in December 2020. Most importantly, the report is an indicator that WPC is making tangible improvements in care coordination and continued investment in this population is necessary to ensure high-quality care for those who are most vulnerable.
For more information on Whole Person Care, see our website.